Saving private healthcare after the verdict
Introduction
“It’s really hard to design products by focus groups.
A lot of times, people do not know what they want until you show it to them.”
– Steve Jobs, CEO, Apple Computer, Inc.
Contrary to some views, healthcare is not a right, but it is the right thing to do. If healthcare is a right, then healthcare professionals become subordinate to that right; and since government controls and enforces rights, the delivery of healthcare would then become healthcare by force. Obamacare is healthcare by force.
Healthcare is, however, the right thing to do. When a doctor happens upon a person bleeding on the sidewalk, he or she is taught that it is the right thing to do to care for that person. This does not mean that the doctor has to care for them, but they will. Why? Making someone else feel better is a caring act and caring is an intrinsic part of medicine. Once you switch from caring to enforcement, medicine becomes forced labor. On the other hand, when you combine caring for others’ health along with free-market principles, you now have the most efficient and beneficial way to deliver the most amount of medical care to the most people.
In an ideal world, prices in healthcare should be a reflection of the perfect balance between the minimal needs of a business given competition and other operating pressures vs. the extra cash the consumer can afford to spend on the healthcare they need.
But to make this work, WE the consumer must deal directly with the doctor or hospital and make every cost and spending decision ourselves, not some health-insurance person and not some faceless bureaucrat. This means that all healthcare dollars must flow through our bank or credit card account and WE should be responsible for whatever is remaining. If we can accomplish this in healthcare, prices will drop — a lot.
McKinsey & Company, a well-respected consulting firm put it this way when discussing the issues in our healthcare system, “The crux of the problem is a mix of high transaction costs and the lack of an efficient way to make consumer-to-provider payments.” (1).
You have seen the seven freedoms of healthcare, commonsense freedoms that will return control of our decisions directly to those of us who need healthcare and those of us who provide it. By combining these freedoms with the free-market structures of other industries, we can now undo years of government intrusion and rebuild the financial structures of healthcare into a complete free-market industry while maintaining the healthcare entitlements we have paid into and we expect.
Here’s another great quote from Dr. Lee Hieb:
“Medicine is a sacred relationship between a physician and a patient — not a relationship between a physician, a government bureaucrat, and a patient.”(2).
The initiative
I, therefore, announce “The Saving Private Healthcare Initiative to restore free-market principles to all healthcare sectors in America”
The Saving Private Healthcare Initiative (“The Initiative”) is not a simple modification of what we have today. It is not a tweaking or a single good idea. The Initiative is a complete overhaul of the financial burdens and risk elements in healthcare that are driving this industry to collapse. The Initiative is not just a great proposal that we hope our federal legislators will decide to add to their legislative agenda. The Initiative includes a bold, action-oriented, all-encompassing plan for all United States consumers, all medical-care providers, health insurance, pharmaceutical and other supporting industries, the current United States Congress and the president. All are key players saving our healthcare system from collapse.
First and Foremost: the Initiative will make certain that the Obamacare bill is completely eliminated. It is a bad law. Its primary goal is to remove healthcare freedom from American citizens and, instead, gives the government massive control over our day-to-day lives and control over our political decisions. But no matter what happens to Obamacare, we must move forward with the reforms of The Initiative.
Conversion to a Free-Market Healthcare System: the Initiative will convert our managed-care system to a free-market system in healthcare, freeing consumers from the heavy burden of highly inflated costs; it will free doctors to practice medicine they way they were taught in medical school. It will free consumers to make informed choices about who will care for them and how much their care will cost. It will free doctors and hospitals from financial restrictions so they can be fully paid at the time of service. The Initiative will also free the government from the healthcare cost burdens that have existed for dozens of years, while improving the quality of care and access to care for those in Medicare, Medicaid and for the uninsured. And finally, the Initiative will bring stability and simplicity to private health insurers so they can deliver improved benefits to their members with reduced risk to their organizations.
In this book, I have outlined the structure of The Initiative in order to give you a general sense of what must be done to fix the financial problems in healthcare. This structure will be used as the foundation to redesign and rebuild the system of who sets prices, who buys, who sells, who pays and how they pay. These changes will ultimately become the foundation of a comprehensive plan for the industry that will include eliminating old financial structures and replacing them with new ones.
Those who do support free-market healthcare, your input will be welcomed. Those who support government-controlled healthcare, your input will not be considered. The Initiative will have open and honest communication with the public, however some communication from The Initiative will be withheld during design phases in order to avoid misleading the public and we will not disclose personnel related matters.
The doctor-patient relationship will be at the core of this effort, therefore the influence of the decision-making process will first come from the consumers of healthcare, second the doctors and the rest will be private hospital representatives, private-health-insurance representatives, those representing other private-healthcare sectors, free-market economists, etc.
It is time for those in our private-healthcare system to fix healthcare. At the end of the day, only we the people can fix our healthcare system. It is too complex for government alone to solve. Been there, done that. We the people respectfully ask Congress and the Administration to take a back seat to re-designing healthcare, so that the private sector can do the job of bringing down costs and regulatory barriers without the influence of special interests and lobbyists. Commonsense, ingenuity and private-market leadership must be our guides in this effort.
In order to implement the new financial structure of healthcare, The Initiative will author the necessary federal and state legislation with ongoing input from our elected representatives. Once completed by The Initiative, the bills will be formally presented to those same representatives for passage and signature to become law. You can think about this process as simply relocating the “sausage making” negotiations from politicians to the private sector.
How big should healthcare be?
According to the website Medica.com, our healthcare industry comprises over 700,000 physicians, 5,200 hospitals, with about 3.8 million inpatient and 20 million outpatient visits per year (3). If you total up all hospitals, clinics, medical professionals, pharmaceuticals, Medicare, Medicaid, nursing homes, dental care, etc., we will on pace to spend about $3 Trillion on healthcare in 2013 (Figure 1).
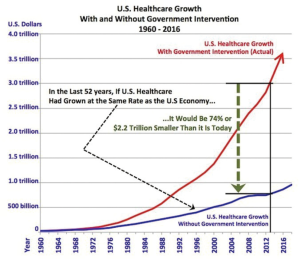
To answer the question, “How big will healthcare be,” it is reasonable to apply a standard growth rate to U.S. healthcare from before the advent Medicare and Medicaid and before managed care. I chose 1960 as the starting point because it was a few years before Medicare was born.
The U.S. economy has grown an average of 6.64% per year from 1960 to 2012. Healthcare has grown an average of 9.37% per year during the same period. That extra 2.73% per year for 52 years adds up to a healthcare industry that is $2.2 trillion larger than it should be. Had Congress and the president not interfered with the free market in healthcare starting with the advent of WWII, we would have an industry that looked more like $767 billion per year, not the $3 trillion it is today. The real question is: can we turn back the clock and remove that extra 74%?
Those who oppose true healthcare reform will argue that the growth in healthcare costs has been due to innovation, and that if you deflate prices, you will lose innovation. Baloney! I strongly argue that the information-technology industry has had as much if not more innovation than healthcare, resulting in decreased prices and increased value. If it can be accomplished in information technology, it can be accomplished in healthcare.
The detractors also argue that you could not cut the financial size of healthcare that much without severely crippling the quality of care and access to care. I believe that The Initiative will, in fact, be able to cut the financial size of healthcare by 67% (in today’s dollars) over a handful of years, which will be gradual enough as to not reduce the quality and access to care. Further, I believe the quality and access to care will increase as a result of The Initiative.
Why 67% and not 74%? I believe that after The Initiative is fully implemented, 7% of the healthcare industry will not experience competitive pressures necessary to cut costs.
What would true, free market healthcare look like?
Before I get into the details of The Initiative, I thought you might like to see how free-market healthcare would work in both a typical doctor’s office visit and in a visit to the emergency room. First, I need to set the stage.
Free-market healthcare means that John and Jane needed to switch from John’s employer-provided health insurance to buying health insurance themselves. They searched hundreds of free-market health-insurance companies (FHICs) across the country and found a policy that they could customize to fit the medical needs of their family. They now possess planned, unplanned, and catastrophic coverage, which offers more coverage than they had under the old “managed-care” model while costing only one-third as much.
Since John and Jane both have full-time jobs, their companies are now depositing monthly benefit-support payments into their new Medical Escrow Account (MEA) at their local bank. They like the fact that the premium payments they make to their FHIC are not taxed as income.
Free-market healthcare: a typical doctor’s office visit
Jane wakes up one morning with a sore throat and aches all over. She has an out-of-town trip planned for later in the week, so she really prefers to see a doctor right away. She gets on the Internet and signs on to their FHIC’s website. She knows they purchased “planned” coverage for their family, so the visit to the doctor will be covered. She then goes to the doctor/hospital search page. She likes the fact that she can search for any medical provider in the country using the Internet. However, if she is not near her computer or does not have a computer, she can use the 1-800 number her FHIC provided, and someone will help her find a doctor right away.
On the search page, she clicks a few drop-down boxes to find the kind of doctor she requires. This just takes a minute or two. A screen is displayed showing all of the doctors in her local area that can treat her. Each doctor is listed with the estimated price for the exam she needs.
Jane typically visits Dr. Jones because she likes the attention she gets from his office and that his services are competitively priced. She remembers checking his credentials when she first started visiting his office. She sees that Dr. Jones charges $40.00 for a cold/flu exam. The website shows that her FHIC policy will cover 75%, or $30.00, for that exam, so she knows that she will need to pay $10.00 after the appointment.
Jane likes the fact that she already knows how much her appointment will cost before she confirms it. She also knows that she could have chosen a less- or more-expensive doctor, which would have cost her less or more out of pocket.
After she selects Dr. Jones, she is then taken to his office’s calendar page showing his availability. For all cold/flu exams, Dr. Jones office recommends it will take 20 minutes. So Jane selects an open time slot that works for her schedule and clicks on the “Make the Appointment” button.
Once the appointment is made, Dr. Jones immediately receives an email from Jane’s FHIC, which gives the doctor a link to access Jane’s electronic medical record. She likes that her medical record is electronic and immediately available via the Internet to any doctor she may have chosen. She also likes that the doctor’s access to her record will only last for a few days after her appointment for data-security reasons.
Jane then heads over to Dr. Jones’s office. In the reception area, they ask her to swipe her healthcare credit card, which had been issued by her FHIC when she and her husband purchased their policy. Her healthcare credit card happens to be a Discover but could have been a MasterCard®, Visa, or American Express. Jane knows that her card can only be used for medical purposes; it will work at any emergency room or at any medical facility where she has made an appointment. She likes this level of security.
Dr. Jones’s office person swipes her healthcare credit card, which puts a hold on $40.00, exactly the fee amount she saw on the Internet.
She has her exam, and the doctor determines she may have strep throat. So he asks if he can perform a strep test, and he looks up this test on his computer. He finds out it will cost her an additional $10.00 and that her FHIC will pay $5 of that. She gives her approval by doing an electronic signature on the computer in the exam room and then he performs the test.
Dr. Jones also wants to prescribe Jane an antibiotic. He enters his preference into the FHIC system, and then it shows all alternative medications and their costs at local pharmacies, including the one that Jane frequents. She and Dr. Jones discuss which medication would be best for her situation, have the fewest side effects, and meets the price Jane is willing to pay. They both agree on an antibiotic that costs $15.00 at the nearby CVS Pharmacy; her FHIC will cover $10.00 of that amount. Again, she gives her electronic approval. The prescription order is made and is electronically sent to CVS.
The total doctor’s bill comes to $50.00 for the exam and the strep test. The office person confirms the credit transaction on Jane’s healthcare credit card, which immediately pays the doctor $50.00. Jane’s portion of the bill is only $15.00, so an electronic notice is sent to her FHIC, which then sends the insurance coverage amount of $35.00, which is debited to her healthcare credit card, leaving a balance due at the end of the month of $15.00.
Jane then heads over to her pharmacy and uses her healthcare credit card to charge her medication. They swipe her healthcare credit card, and it charges $15.00 to CVS Pharmacy; her portion of the total is $5, so her FHIC immediately debits $10.00 back on her card, leaving a balance due at the end of the month of $5.00.
A few weeks later, she gets the bill from her healthcare credit card company. She sees a credit charge of $50.00 paid to Dr. Jones and a debit charge of $35.00 from her FHIC, which leaves her responsible for a $15.00 balance. She also sees a credit charge for CVS Pharmacy of $15.00 and a debit charge of $10.00, leaving her to pay $5.00.
So the total out of pocket cost for Jane’s visit to her doctor and pharmacy is $20.00, which she pays to the Medical Care Credit Card Company.
Free-market healthcare: an emergency-room visit
John and Jane’s son Jake is playing soccer with some relatives while they are on vacation. Jake has a hard fall, and they suspect he has a fractured arm. John takes him to the closest emergency room. The hospital requests John’s healthcare credit card and swipes it, putting a hold amount of $500.00 (the amount the hospital estimates it will cost to treat a possible fracture). Using the information on John’s healthcare credit card, the ER nurse goes to the Internet and to John’s FHIC website to open up Jake’s electronic medical record.
The doctor examines Jake and finds out that he does indeed have a hairline fracture. They treat his arm, giving him some medication for pain and applying a cast. The total amount they charge is $350.00, which is put on John’s healthcare credit card. Since all medical visits are paid for on a time-and-materials basis, their costs were less expensive since it took less time to treat Jake’s arm than anticipated.
Since John and Jane purchased “unplanned” insurance from their FHIC, their policy covers 80% of the ER cost. So after the $350.00 charge is applied to their healthcare credit card, an electronic notice is sent to their FHIC, which debits John’s card for $280.00. John knows he will need to pay $70.00 to the healthcare credit card company when the bill comes in at the end of the month.
These two examples cover most of the changes in free-market healthcare from a patient point of view. In the following pages, this book will cover all the major areas of healthcare and how The Initiative will apply these free-market principles, resulting in a more streamlined healthcare financial system and a dramatic lowering of costs.
The ten major reforms of the initiative
Since price controls and political coagulation got us into this mess, we need to break the coagulation (eliminate all provider-payer contracts), stop all forms of price controls and all forms of managed care. We need to put the consumer directly in control of every insurance and medical-care decision because they are the ones most affected by them. Most importantly, all medical-care providers need to advertise all of their fees, become quality and price competitive and they need to be paid 100% of their advertise fees at the time of service.
Here is a list of the 10 major reforms built into the Initiative. They will be explained in detail in the remaining chapters of this book and are not chronological.
(I) Separating the Three Titans of Healthcare: the Initiative financially separates the three titans of healthcare: (i) Government healthcare agencies, (ii) Health-insurance companies and (iii) Medical-care providers. Nearly all in each of these groups are connected by contracts. The Initiative cancels all of these contracts and contractual relationships.
(II) Free-Market Health Insurance: the Initiative converts all managed-care health-insurance companies to Free-Market Health-Insurance Companies (FHICs) by making the following changes:
— Converts all health-insurance companies from selling healthcare policies through employers to selling healthcare policies directly to consumers.
— Requires the elimination of all managed-care functions within private-health-insurance companies.
— Requires all medical-care providers to relocate the medical records for their patients to each patient’s free-market health-insurance company who will convert them to a standardized electronic form or EMR. Medical-care providers will be able to retrieve these records only via the secure Internet.
— Requires that all health-insurance companies create a new Internet-based Provider Search and Appointment Scheduling (PSAS) system that will give their members the ability to search for any medical-care provider and show all medical fees, costs and amounts of coverage before the appointment is made. This same system will also give consumers the ability to schedule their own appointment with the medical-care provider they have chosen. Medication options, pricing and selection by doctors will be included as well. For those who do not have access to the Internet, FHICs will provide 1-800 phone service, which will have representatives provide the same functions.
— Recommends three types of policies for health-insurance members: planned, unplanned, and catastrophic. Planned pays for any medical care when the previous search and selection system is used. Unplanned pays for mostly emergency-room visits and catastrophic coverage pays for high-cost medical care.
— Direct-Pay Medical Services: with deductibles becoming so high these days, people are looking to reduce the cash-shock that comes when needing medical services. Direct-pay medical services are annual contracts that you or your family establish with a small group or large network of physicians in your area. The monthly costs are usually below your employer’s health plan annual deductible and allow you to pay a flat, low-cost monthly retainer fee. Some call these “physician-retainer” services. Since direct-pay organizations cover costs in the deductible portion of your current health-insurance plan, they are considered to be complimentary to the health-insurance industry.
— One service that has been up and running for several years covers your day-to-day medical needs in physician offices and in hospitals. Excluded are catastrophic care, emergency-room charges, hospital facility charges, long-term care and out-of-town medical charges. The monthly cost can be as low as a few hundred dollars per month to get access to a local network of more than 100 of physicians. If your preferred physicians are not on the list, you can request they be added. There is little to no risk for the physician to sign up. This type of service gives you and your family freedom to access any of the physicians in your network, any time they are available. No co-pays, no deductibles, no appointment bills. Please see the website www.savingprivatehealthcare.com for contact information.
— The Initiative recommends several enhancements to these types of medical-service organizations. A simple PSAS system would be helpful to their members showing each physician’s monthly retainer fee, so customers can price-shop different physicians. The Initiative also recommends one EMR system per organization be established to relieve those physician practices from maintaining expensive EMR systems and to allow the customers to switch between physicians in their network without having to worry about how to move their medical records from one office to the next. Finally, a prescription-drug-selection capability is recommended so that the physician can show their patient their recommended medication, substitute medications and the costs of each at multiple local pharmacies.
(III) The Medical Escrow Account: the Initiative establishes the Medical Escrow Account (MEA), a new type of account to be available at all U.S. banks. The MEA will receive monthly healthcare-benefit payments from employers, consumers (MEA account holders) and Medicare. The MEA will be used to make tax-deductible health-insurance premium payments or direct medical-care payments, over a person’s lifetime.
(IV) Eliminating Price Controls: the Initiative removes all medical fees determined by health-insurance companies, Medicare and Medicaid, leaving all doctors & hospitals to set their own prices with a more simplified format that is easier for consumers to understand.
(V) Free-Market Medical Fees: the Initiative will require the medical community develop a brief list of consumer-friendly procedures. It also requires that all medical-care providers develop their own single set of estimated fees based on time and materials rather than per-procedure. These procedures will be easily selectable via the Internet on every FHIC’s PSAS system, which will then display the associated fee(s). As mentioned, The Initiative also removes paper charts and electronic medical records from physician offices and moves them to their respective health-insurance companies as electronic medical records to be securely accessed by only authorized medical-care providers, anywhere.
(VI) Free-Market Medical Care Credit Cards: the Initiative requires that all patients pay 100% of their medical fees to their medical provider at the time of service. To accomplish this, The Initiative establishes fixed, low-interest Medical Care Credit Cards (MasterCard®/VISA/Discover, American Express, etc.) for FHIC members. These credit cards can only be used to pay for medical-care needs at the time of service. All covered amounts are to be debited onto the card and the insured member pays the balance at the end of the month or over time as a revolving balance.
(VII) Medicare-Private: many seniors are concerned about the future of Medicare. The Initiative removes that fear by maintaining the federal guarantee of medical care health insurance, increasing the quality of care received by seniors and decreasing the cost of their medical care. These changes will ensure that Medicare is not only around for generations to come, but will become a much stronger program in the future.
— The Initiative converts Medicare into Medicare-Private, a complete private-healthcare-industry benefit-support program offered under Medicare that will eventually combine Medicare Part A, Part B, Part C, Part D, and Medicare Advantage plans into the single, Medicare-Private plan. Medicare Supplement Plans will no longer be required. Medicare-Private removes all Medicare managed-care functions, all mechanisms that determine medical fees, and the need for any provider fraud investigation functions.
— Medicare-Private combines the major Medicare programs over time into a simple organization that deposits monthly benefit-support payments into all recipients’ Medical Escrow Accounts. These payments will enable all seniors, in all areas of the United States to choose and purchase affordable health-insurance plans from FHICs.
(VIII) Medicaid-Private: the Initiative converts Medicaid into the Medicaid-Private program which makes the following changes:
— Federal Changes: removes all current federal Medicaid spending decisions. Each state will be able to spend their Medicaid funds as they see fit. This will be accomplished by block grants provided by the federal government to each state based on need for those funds.
— Additional State Medicaid Changes: recommends the removal of all state Medicaid managed care functions, all mechanisms that determine medical-care provider fees and all fraud investigation functions.
For inpatient, long-term and nursing home care needs of Medicaid recipients, each state should establish a PSAS system to manage the selection of low-cost medical-care providers. Caregivers would use PSAS to select the lowest-cost medical provider in their area and would be given Medical Care Debit Cards to be used for their recipients. Audit trails be produced by the PSAS system and sent to their Medicaid Administrators to assure the lowest-cost providers are being selected according to policy.
(IX) Free-market Healthcare for Those in Need: for the millions that do not have any form of insurance or for those who do have insurance but do not have the money for the out-of-pocket costs, The Initiative has several avenues to help relieve the financial burdens they face.
— The New Jersey Solution: there is a bill currently pending before the statehouse in New Jersey that has strong bipartisan support and addresses a large portion of the medical needs of the uninsured and Medicaid recipients.
Here is a quote from Dr. Alieta Eck, President of the Association of American Physicians & Surgeons, who is playing a major role in supporting this bill:
With this bill, medical-care providers will have the opportunity to establish free clinics in low-income urban or rural areas and each donate four hours of their time per week to these clinics. Experience has shown that the average cost per medical appointment in these clinics is only $13.00 and supportable by cash-box donations. In exchange, the state will obtain complete medical-malpractice protection for these physicians through the federal government under the Federal Tort Claims Act. Thus, if a patient believes he or she has been wronged by a physician who volunteers, they will be required to direct their claim to the state.
This program will address most medical care for the needy and will replace up to half of all Medicaid health costs for each state with the exception of inpatient, long-term and nursing home care needs.
— Donation Care: for those who are not insured and who need inpatient hospital care, The Initiative will ask hospitals to set up donation care computer systems to route the donation care to where it is needed the most. Physicians who donate four hours per week plus this computer system should be able to handle nearly all uninsured patient situations.
The Initiative supports legislation for the IRS to make all donation care 100% tax-deductible on personal federal tax forms. Medical professionals may opt to donate more or less than the four-hour target.
— Low-Interest Medical Loans: for those few patients who are uninsured and still have a balance remaining at a hospital or doctor’s office, then prior to discharge they will be required to establish a fixed, low-interest Medical Loan, which will be guaranteed by the United States government and sponsored through any U.S. bank. Banks and other financial institutions can work with the borrower to offer longer-term payouts and special financing as needed.
(X) Eliminating Defensive Medicine: the aforementioned New Jersey Solution will address most of the defensive-medicine issue in each state that passes a similar law. Medical-malpractice claims have to be filed with the state vs. against the physician. This should dramatically decrease the number of frivolous medical lawsuits and address most of the need for physicians to practice defensive medicine. The Initiative will monitor the success of this program in New Jersey and may make additional recommendations to eliminate defensive-medicine once and for all.
These 10 major reforms of The Initiative along with additional reforms described in later chapters will stop and reverse the upward spiral of inflation in healthcare, resulting in a gradual but highly effective 67% reduction in overall healthcare costs. I have more details about these reforms and cost reductions later in the book. These reforms remove waste and open up price competition for providers in order to drive down prices throughout nearly all aspects of healthcare. These reforms will also reduce the financial and legal risk of practicing medicine, which is key to eliminating unnecessary and overly costly medical treatments.
Freedoms restored with the initiative
The consumer will now be free from the cost burdens that have plagued healthcare for many decades. They will now be able to choose from every doctor, hospital or other medical facility for each and every medical need they have. They will have the freedom to choose from every health-insurance company and plan, and they can keep their health-insurance policy before, during, and after turning sixty-five, which virtually eliminates the problem of pre-existing conditions. They will also have the freedom to choose a customized health policy based on the medical needs of their family, and they will have the freedom to know how much their medical care will cost and how much insurance will cover before their appointment or procedure.
Medical-care providers will be free from all provider contracts so they can deliver medical care without obligations to health-insurance companies, Medicare, or Medicaid. They will be free to run their businesses as they see fit (within medical practice safety, quality and ethical guidelines), and they will be free to compete with one another based on the quality of care they provide and prices they charge. They will no longer incur the business risk of paying for expensive electronic medical records systems. Doctors will have a lower financial risk due to lower medical-malpractice premiums, and they will have more freedom to practice medicine as they were taught in medical school and not as some health-insurance manager, government bureaucrat, or attorney dictates.
Private-health-insurance companies will be free from having to face a collapsing industry due to the out-of-control price spiral and Obamacare. They will also be free from the cost burden of having to manage provider contracts, provider lists, and health utilization.
The federal government will be free of the massive cost burdens presented by Medicare and Medicaid and will no longer have to institute things like the “doc-fix” and other patchwork measures to keep doctors from leaving Medicare. And finally, state governments will be free of the massive cost burdens associated with managing their Medicaid plans.
Building and implementing the initiative
We have all seen a number of ideas as to how to reform healthcare in the United States Books have been written, legislation proposed, and several major healthcare bills signed into law. All of these efforts have failed on several fronts. First, if we are ever going to get true and beneficial healthcare reform, it must be born in the private sector and fully developed by the private sector. With healthcare’s size and complexity, no one person (certainly not I) and no one set of legislators can fully understand the detail of what needs to be done to reform healthcare properly. Second, most previous reform efforts that go through the legislative process may start out as good ideas, but our politicians are beholden to many powerful political forces that take control of the reform legislation and redraft it to benefit certain political groups to the detriment of the healthcare system itself. This is counter-productive and potentially catastrophic, as we have seen with Obamacare.
To address these shortcomings, I will create a temporary launch committee in 2013 whose job it will be to select the leadership of The Initiative. All members of The Initiative will have short tenures, and well-established procedures for their replacement. This will prevent political coagulation.
I will not accept an employed or voting position in the Initiative because this will create a conflict of interest; however, I will accept an advisory role if offered.
Both the launch committee and the leadership of the Initiative will be comprised primarily of consumers and doctors, then secondarily by representatives of the other major healthcare sectors, including a few outside experts.
The Initiative will use this book as an outline of what must be done to achieve free-market healthcare in this country. There will be The Design Initiative, the Legislative Initiative, and the Implementation Initiative. Due to the huge amounts of money and political influence involved, this group will work diligently to prevent any conflict of interest by avoiding two-way governmental contact during the design stage; however, input will be welcomed from all free-market healthcare supporters. When we move into the Legislative Initiative, we will open up two-way communication with legislators to gain the votes necessary for passage of our bills.
In the design phase, the Initiative will actually create the entire reform plan for all sectors of the healthcare industry, both private and public. As this plan is being developed, The Initiative will also draft seven free-market healthcare bills, as I have outlined in Chapter 17.
Once The Design Initiative is complete, the Legislative Initiative will begin. Two-way governmental contact will then be initiated to gain the votes needed for passage of these bills. All changes to these bills in this stage will be made publically available, including the reason(s) for the changes. No backroom deals will be permitted.
Once enough votes are secured for each bill, they will be formally presented to Congress and the president for passage and signature without amendment. The Initiative will have already included all necessary changes.
As each of the seven bills of The Initiative are passed and signed into law, The Implementation Initiative will begin. By 2022, free-market healthcare will be fully implemented.
At this point, the vision of true free-market healthcare will be realized. As a result, The Initiative and all its members will permanently disband. Private Healthcare will be saved.
Assuming no legislative or other delays, from launch to completion it is anticipated that The Initiative will be completed by 2022.
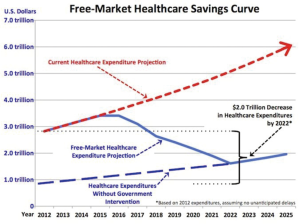
$2 Trillion cost savings by 2022 (1)
Free-Market healthcare’s cost savings will come from a number of areas of the healthcare industry. Here is a high-level breakdown of the estimated savings as The Initiative is fully implemented (Figure 2):
With a goal of $2 Trillion in cost reductions* I have estimated the savings to come from the following areas:
Medical Provider Cost Savings $1,774 Billion
—Reduction of $750 Billion: Defensive Medicine Elimination
—Reduction of $552 Billion: Increased Medical Provider Price Competition
—Reduction of $247 Billion: Managed-Care Elimination
—Reduction of $205 Billion: Other Provider Administration Efficiencies
—Reduction of $16 Billion: Medical-Malpractice Premium Reductions
—Reduction of $4 Billion: EMR Systems Moving to Insurance Companies
Healthcare Insurance Cost Savings $61 Billion
—Reduction of $52 Billion: Insurance Administration
—Reduction of $36 Billion: New Health-Insurance Competition for Consumers
—Increase of $22 Billion: Adding Cost for New Medical Care Credit Cards
—Increase of $5 Billion: Adding New EMR & PSAS Systems
Pharmaceutical Cost Savings $150 Billion
—Reduction of $150 Billion: Increased Pharmaceutical Price Competition
Government Healthcare Administration Cost Savings $15 billion
—Reduction of $15 Billion: Government Administration
Total Annual Free-Market Healthcare Cost Savings $2,000 Billion (US)
Medicare, Medicaid Cost Savings: these programs are mostly “pass-through” programs, meaning that the medical-care costs saved will pass from the medical-care providers through to the respective government agencies. However, for the governments involved with these programs, I have projected the cost savings of free-market healthcare. Note that these costs savings are inclusive of, not additive to the above numbers.
Medicare Cost Savings: medicare-Private will reduce healthcare outlays as the cost as medical care comes down, saving the federal government approximately $400 billion per year (in 2012 dollars). Please note, these are not, “cuts” as politicians like to say. Not one dime of money will be “cut” from Medicare. Costs will decrease as medical care costs come down, maintaining as good or better healthcare quality for all Medicare members.
Medicaid Cost Savings: medicaid-Private will reduce healthcare outlays as the cost as medical care comes down, saving state/federal governments approximately $231 billion per year (in 2012 dollars). These savings assume that all states adopt The Initiative’s free-market healthcare structure as soon as the implementation schedule permits.
I do anticipate the Congressional Budget Office (CBO) will generate a different set of numbers. If their estimates are based on the legislation as written by the Initiative, they will be close to the summary numbers above. If however, the political process alters the Initiative’s healthcare-reform legislation, I cannot predict what the CBO estimates will be.
Acknowledgment
I would like to first give my thanks to my incredible wife Kate for her advice, patience and knowledge of the healthcare industry. You were always in my corner, even when the room was round. I would like to send a special thanks to our terrific kids: Andrew, Chris, Jenna and Kristen. Thanks to Pastor Glen and Jimmy Zawiski who guided me when I needed it the most.
I would also like to thank Dr. Alieta Eck of the Association of American Physicians and Surgeons for her contribution to this effort and her tireless work for those who cannot afford medical care. Thank you to Dr. Loel Fenwick and Dr. Rich Sugden for their experience and robust efforts in supporting free-market healthcare, and to Dr. Adrienne Cresswell and her direct-pay organization.
I would like to again thank my wife Kate, and to Jimmy Zawiski, and Joanne Asala of Compass Rose for their terrific editing; my good friend, Donna Wilson for her great illustration work and Sarah Evans of Sevans Strategy for her great now-knowledge of the social world.
To all the medical professionals out there, you’ve saved my life several times over. I owe you my thanks and a debt of gratitude that can never be repaid. And, most honorably, I thank God for patiently giving me what I needed to write and complete this book.
Disclosure: This publication is designed to provide accurate and authoritative information in regard to the subject matter covered. It is sold with the understanding that the publisher is not engaged in rendering legal, accounting, or other professional services. If legal advice or other professional assistance is required, the services of a competent professional person should be sought.
— From a Declaration of Principles jointly adopted by a Committee of the American Bar Association and a Committee of Publishers and Associations.
No responsibility or liability is assumed by the publisher for any injury, damage, or financial loss sustained to persons or property from the use of this information, personal or otherwise, either directly or indirectly. While every effort has been made to ensure reliability and accuracy of the information within, all liability, negligence or otherwise, from any use, misuse, or abuse of the operation of any methods, strategies, instructions, or ideas contained in the material herein, is the sole responsibility of the reader.
Copyrights not held by the publisher are owned by their respective authors.
All trademarks and brands referred to in this book are for illustrative purposes only, are the property of their respective owners, and are not affiliated with this publication in any way. Any trademarks are being used without permission, and the publication of the trademark is not authorized by, associated with, or sponsored by the trademark owner.
All information is generalized, presented for informational purposes only, not given as medical advice, and is presented “as is” without warranty or guarantee of any kind. Readers are cautioned not to rely on this information as medical advice and to consult a qualified medical, dietary, fitness, or other appropriate professional for their specific needs.
This information has not been evaluated by the FTC or any other government agency; the information is not intended to “diagnose, treat, cure, or prevent any disease.”
All information and resources found in this book, on the or websites, on blog support groups, or in additional publications by this author, (Materials) are for educational purposes only. These Materials are not licensed medical professional resources, therefore the author and publishing company do not render medical advice or professional services. Information contained in the Materials should not be used to diagnose or treat any health problems, concerns, or diseases. The information in the Materials is intended, but not promised or guaranteed, to be correct, complete, and current and is not meant to substitute for the advice provided by your own physician or other medical professional. You should not use the information contained herein for diagnosing or treating health problems or diseases, as only a licensed physician or medical professional can do. If you have a specific medical condition or concern, please contact your local healthcare professional. If you have a medical emergency, please contact your local 911 or emergency healthcare system.
All information, opinions, comments, or provided material are copyrighted material.
Saving Private Healthcare The inclusion of any and all information in is not to be implied as endorsements, and there is no fee or financial compensation for placement in this publication.
References
- Nick A. LeCuyer and Shubham Singhal, “Overhauling the U.S. Healthcare Payment System,” McKinsey & Company, June 2007. Available online: https://www.mckinseyquarterly.com/Overhauling_the_US_health_care_payment_system_2012
- Dr. Lee Hieb, “Why AAPS? Message from AAPS President Lee Hieb, M.D.,” September 26, 2011, AAPSOnline.org. Available online: http://www.aapsonline.org/index.php/site/article/why_aaps_message_from_aaps_president_lee_hieb
- The Medica Website, “Medical Industry Overview” Retrieved August 1, 2012. Available online: http://www.themedica.com/industry-overview.html
- Centers for Medicare and Medicaid Services, “National Health Expenditures Aggregate, Per Capita Amounts, Percent Distribution and Average Annual Percent Change: Selected Calendar Years 1960–2010, Retrieved 06/02/2012. Available online: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical.html
- Allcountries.org Website, “National Health Expenditures by Type,” Retrieved on June 2, 2012. Available online: http://www.allcountries.org/uscensus/151_national_health_expenditures_by_type.html
- U.S. Bureau of Economic Analysis, Retrieved August 11, 2012. Available online: http://www.bea.gov/national/xls/gdplev.xls