Obstructive jaundice suspected hilar cholangiocarcinoma
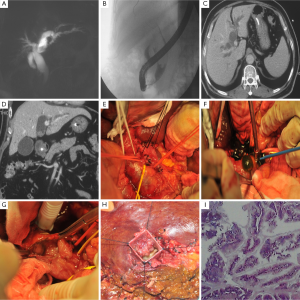
A 60-year-old man was admitted to our department for presenting with jaundice for 20 days. His past history was unremarkable. On physical examination, gallbladder was enlarged and palpable under the right coastal margin; however, Murphy’s sign was negative. The laboratory tests revealed abnormally serum levers of the total bilirubin of 76.8 µmol/L with direct-reaction fraction of 52.3 µmol/L, alanine aminotransferase of 188 U/L, alkaline phosphatase of 248 U/L, gammaglutamyl transpeptidase of 759 U/L, and aspartate aminotransferase of 99 U/L. Tumor marker tests showed serum carcinoembryonic antigen and alph-fetoprotein were within normal ranges, but serum carbohydrate antigen (CA) 19-9 lever was slightly elevated (53.9 U/mL). Serology was negative for hepatitis B and C. Abdominal magnetic resonance cholangiopancreatography (MRCP) revealed markedly dilatation of the common bile duct (CBD), 2.3 cm in the greatest diameter but normal pancreatic duct (Panel A); a spacing-lesion at the proximal of the left hepatic duct (LHD) was found. Endoscopic retrograde cholangiopancreatography (ERCP) showed an irregular filling defect within the middle part of CBD and proximal part of CBD could not be adequately visualized (Panel B). Intraductal ultrasonography (IDUS) revealed the walls of the CBD intact and there were a lot of moderate-high echoic things within the lumen of CBD. Much of dark green mucinous liquid was removed repeatedly through the CBD. Computed tomography (CT) scanning revealed intrahepatic, extrahepatic bile ducts dilatation and gallbladder distension (Panels C and D); multiple hypodense lesions with slightly enhanced were seen within common hepatic duct (CHD) and CBD. With a suspicious diagnosis of hilar cholangiocarcinoma, a laparotomy was performed under general anesthesia. During operation, a distended gallbladder, dilated CHD and CBD were found (Panel E). No abnormal lesions in liver and enlarged lymph nodes in helium were detected. With open CBD exploration, a lot of dark green of mucinous material flowed from CBD (Panel F). The result of CBD exploration identified these of mucinous materials originated from the LHD (Panel G). A cholecystectomy and a left hemihepatectomy with T-tube placement within the CBD were then performed. On the gross examination of the resected specimen, a papillary neoplasm could be found within the originating part of lumen of the LHD (Panel H). Histological pathology demonstrated the surgical specimen was an intraductal papillary mucinous neoplasm of the bile duct (Panel I); the neoplasm invaded LHD and its bile tree; and surgical margin was negative. His past-operative period was uneventful, and the patient discharged on the 16th past-operative day. He did not accept any further anti-cancer therapy.
Acknowledgements
Disclosure: The authors declare no conflict of interest.