Laparoscopic first step approach in the two stage hepatectomy
Introduction
Resection is the gold standard therapeutic option for patients with colorectal liver metastases. However, only 20-30% of patients are resectable (1). In recent years, different therapeutic options improved the rate of patients eligible for surgery. These results can be obtained with new chemotherapeutic regiments, new biological therapies, and with more aggressive surgical procedures such as the two-step strategy. Since the first two staged hepatectomy reports (2), liver resection indications have been implemented with new surgical procedures. In patients with colorectal or neuroendocrine bilobar liver metastases, two stage hepatectomy is nowadays routinely performed in hepatobiliary centers. In patients with a concomitant future liver remnant (FLR) less than 25-30%, in both the cases of normal liver or liver parenchyma affected by chemotherapy-related damage, a single stage resection is not feasible. In these cases patients need a first stage resection of liver metastases in the left liver with a concomitant portal vein ligation (PVL), and a second stage hepatectomy of the right lobe if the FLR has grown enough. Laparoscopy for liver resections has been demonstrated as a safe procedure in several indications (3-6).
The aim of this study is to evaluate the feasibility and the rates of morbidity and mortality of the laparoscopic approach in the first-step of two stage hepatectomy (wedge left liver resection and right PVL).
Materials and methods
We retrospectively reviewed all the patients undergoing a two stage hepatectomy for bilobar colorectal metastases, all identified from a prospectively collected database. From 2004 to March 2014, 73 patients underwent a two stage hepatectomy: of these patients, 4 underwent a totally laparoscopic first step (liver resection and PVL).
Age, gender, body mass index (BMI), number of lesions, prior surgery, procedure time of first and second stage, length of hospital stay of first and second stage and follow up data were collected.
All patients were studied with a volumetric computed tomography (volCT) before first step and 30-40 days after PVL to confirm hypertrophy of the FLR. Second step was performed only if disease progression was excluded and FLR >30%. In this series no underlined liver disease was observed.
Surgical procedure
Patients were placed supine on the operative table with lower limbs apart, the surgeon between the legs. Access to the abdomen was gained by open technique and pneumoperitoneum was maintained at 12 mmHg. A 10-mm port at the umbilicus housed a 30° video-camera. The other three trocars were positioned usually along a semicircular line with the concavity facing the right subcostal margin. Diagnostic laparoscopy was first performed and lysis of adhesions was performed is necessary. Steep reverse Trendelenburg position was maintained. The liver was examined using laparoscopic ultrasonography (US) to confirm the extension of the lesions and their extension in the left lobe. If operability was confirmed only the right part of the pedicle was dissected. Bile duct was elevated after dissection with the intent to clearly expose the portal vein. Right portal vein was then encircled with loop (when necessary, anterior and posterior vessels were encircled separately). Wedge resection of the left metastases was performed. After completing the resection of left liver metastases, right portal vein was legated with clips or with loop ligation. A perioperative Doppler was then performed in all patients. Thirty-forty days after the first step a volCT was performed. Patients underwent the second step of the two stage hepatectomy if no progression of the disease was observed and the FLR was increased enough.
Results
Patients’ characteristics are resumed in Table 1. All the patients were male. Median age was 55 years. One patient underwent an atypical wedge resection of segments II-III and a laparoscopic PVL (LPVL), one patient had a first wedge resection of segment II and LPVL, and two patients underwent wedge resection of segment III and LPVL. First step surgical mean time was 189 (range, 160-244) min, mean blood loss was 22 (range, 0-50) cc. No transfusion was required in this series. Mean days between the first and second step was 86 days. All second step operations consisted in an open right hepatectomy (RH). Mean surgical time was 304 (range, 260-324) min, and mean blood loss was 425 (range, 200-700) cc. For second step no transfusion was necessary. Length of hospital stay for the first step was 3, 5 (range, 3-5) days, and for the second step 8 (range, 7-10) days.
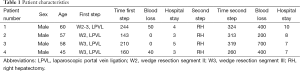
Full table
Discussion
In patients with normal liver, FLR less than 30% is considered a contraindication for surgery. Portal vein occlusion is now currently used to induce hypertrophy of the FLR before surgery. In literature the use of laparoscopy for two-stage hepatectomy has not been discussed enough, only few reports being available. The Southampton experience confirms our preliminary results that laparoscopic approach is feasible (7). However, they reported height cases with only two of them undergoing LPVL. Two studies analyzed the laparoscopic approach for PVL prior to major hepatectomy (8,9). LPVL was compared to portal vein embolization (PVE), showing the safety of LPVL and its ability in inducing an adequate FLR increase. Despite PVE is a less invasive procedure and it has been described as superior to open PVL (10), it is affected by up to 15% of complications (11). In our series no complications were described during the laparoscopic first step procedure. Laparoscopy carries the advantages of few adhesions and shorter lengths of hospital stay respect to open approaches. Another advantage of laparoscopic approach is the rapid patient’s recovery resulting in a short discontinuing of the chemotherapy regimen. The advantage concerning the immunity of laparoscopic approach is suspected but not demonstrated (12).
Conclusions
This study described a first experience of laparoscopic approach for two stage hepatectomy. Although the study included only four patients, which is not sufficient for obtaining any scientific definitive result, the evidences of our study suggest us that the first step of hepatic resection and PVL is feasible with a laparoscopic approach in patients with bilobar liver metastases. This mininvasive laparoscopic approach seems to reduce adhesions and hospital stay and should be proposed in all patients planned for a two stage hepatectomy with bilobar metastases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Abulkhir A, Limongelli P, Healey AJ, et al. Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg 2008;247:49-57. [PubMed]
- Adam R, Laurent A, Azoulay D, et al. Two-stage hepatectomy: A planned strategy to treat irresectable liver tumors. Ann Surg 2000;232:777-85. [PubMed]
- Ettorre GM, Laurenzi A, Lionetti R, et al. Laparoscopic liver resections in normal and cirrhotic livers: a retrospective analysis in a tertiary hepato-biliary unit. Dig Liver Dis 2014;46:353-7. [PubMed]
- Cherqui D, Husson E, Hammoud R, et al. Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg 2000;232:753-62. [PubMed]
- Cho JY, Han HS, Yoon YS, et al. Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 2008;144:32-8. [PubMed]
- Nguyen KT, Laurent A, Dagher I, et al. Minimally invasive liver resection for metastatic colorectal cancer: a multi-institutional, international report of safety, feasibility, and early outcomes. Ann Surg 2009;250:842-8. [PubMed]
- Di Fabio F, Whistance R, Rahman S, et al. Exploring the role of laparoscopic surgery in two-stage hepatectomy for bilobar colorectal liver metastases. J Laparoendosc Adv Surg Tech A 2012;22:647-50. [PubMed]
- Ayiomamitis GD, Low JK, Alkari B, et al. Role of laparoscopic right portal vein ligation in planning staged or major liver resection. J Laparoendosc Adv Surg Tech A 2009;19:409-13. [PubMed]
- Are C, Iacovitti S, Prete F, et al. Feasibility of laparoscopic portal vein ligation prior to major hepatectomy. HPB (Oxford) 2008;10:229-33. [PubMed]
- Broering DC, Hillert C, Krupski G, et al. Portal vein embolization vs. portal vein ligation for induction of hypertrophy of the future liver remnant. J Gastrointest Surg 2002;6:905-13; discussion 913. [PubMed]
- Liu H, Fu Y. Portal vein embolization before major hepatectomy. World J Gastroenterol 2005;11:2051-4. [PubMed]
- Corrigan M, Cahill RA, Redmond HP. The immunomodulatory effects of laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 2007;17:256-61. [PubMed]


