Secondary gallbladder hydatidosis and nonfragmanted germinative membrane sourced obstructive jaundice caused by intrabiliary ruptured hepatic hydatid cyst (a case report): two rare complication of the intrabiliary ruptured hepatic hydatid cyst
Introduction
Hydatid disease is a parasitic disease caused by larval form of the Echinococcus Granulosus. Hydatid disease mainly affects the liver. Hepatic hydatidosis is known as a cystic liver disease since the ancient times.The disease concept caused by the embryonic form of an adult parasite was first described by the anatomist Edward Tyson in 1683 (1). Echinococcus Granulosus is the most common type of echinococci to form the cystic hepatic disease. Sixty-seventy per cent hydatid cysts take place at the liver. In 80% of the cases, the right lobe of liver is affected; 20% of cases affect the left lobe (2). A hydatid cyst is formed by three membranes. The outer pericyst, which is fibrous protective zone, composed of host cells. The middle acellular laminated membrane, the inner germinative membrane where the scolics and the laminated membrane are produced. Last two membrane form the true layers of the cyst. Daughter vesicles are vesicles which are filled with scolics, originated from germinative membrane (2). Hepatic hydatid cysts may remain symptom-free for long years. In 1/3 of cases, complications, such as rupture (intrabiliary, intraperitoneal, intrapleural), abscess, anaphlaxia, sepsis are developed (3).
Case report
A 58-year-old male was referred to our hospital with epigastric pain, jaundice, fever, nausea and weight loss for two months. An epigastric mass of 10 cm diameter was palpated. Increased liver function test levels were revealed by laboratory findings {AST: 54 U/L [5-45], ALT: 78 U/L [5-55], T.bil: 7.4 mg/dL [0-1.2], D.bil: 7.1 mg/dL [0-0.3], ALP: 447 U/L [35-104], GGT: 197 U/L [7-50]}. On abdominal ultrasound, the cystic mass of 10 cm diameter in left lobe of liver and multiple milimetric echogenicities within the gall bladder and a main biliary duct dilation were noted. On MRCP, a lobulated well-defined cystic mass including multiple daughter vesicles and ondulated internal membranes are seen at the left hepatic lobe. Gallbladder revealed many milimetric filling defects. Main biliary duct was dilated and measured 2 cm in diameter and showed filling defects.
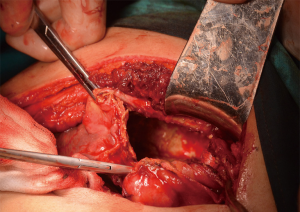
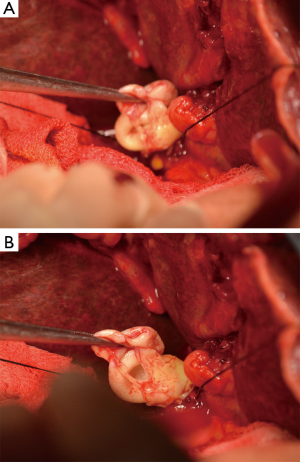
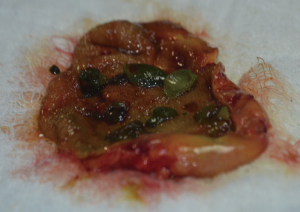
The patient has undergone operation with subcostal incision. A cystic mass in 12 cm diameter in the left lobe of liver was detected. After the hypertonic serum saline infusion into the cyst; cystotomy and cyst drainage were performed (Figure 1). Any connection between the cyst and the biliary tree was not found. Main biliary duct was 2 cm in diameter. Cholecystectomy was performed. There were multiple daughter vesicles in the gallbladder, which were approximately 0.5-1 cm in diameter, were painted with bile (Figure 2). Choledocotomy and choledocus exploration were done. A large germinative membrane and small daughter vesicles which had caused the main bile duct obstruction, were evacuated (Figure 3). Choledocoduodenostomy was performed following the biliary tract lavage to provide the permanent biliary tract drainage and to reduce the mortality and morbidity. After the spontaneously regression of the bile leakage emerged in postoperative period, the patient was discharged and advised to take albendazol therapy for 8 weeks.
Discussion
Intrabiliary rupture of the hepatic hydatid disease is described as the most common complication (5-15%) in different series.Rupture is the result of increased intracystic pressure. Intrabiliary rupture was first reported by Harold Dew in 1928 (4). Intrabiliary rupture of the hepatic hydatid cyst can be frank or occult (5). Frank intrabiliary rupture becomes remarkable with obstructive jaundice, acute cholangitis or acute pancreatitis (6,7). Frank rupture happens to be in 5-15% of the cases (8). Ninety per cent of cases of frank biliary ruptures refer with obstructive jaundice (3). Occult intrabiliary cyst rupture is silent generally and becomes evident with a biliary fistula which occurs during the postoperative period. The drainage of cyst contents into the main biliary duct results in obstructive jaundice and acute cholangitis.
Main cyst components which cause to obstructive jaundice are daughter vesicles, fragments of germinative membrane, hydatid stones and hydatid cast sand. In our case, although any communication between the biliary tract and cyst is not demonstrated intraoperatively, intrabiliary large nonfragmanted germinative membrane is shown to be the main reason of obstruction. As a main reason of this situation, we think that there is a long period of time between the onset of the disease and the definitive therapy. Choledochoduodenostomy is supervened to the operation procedure to prevent a possible biliary fistula postoperatively, because of this reason (6).
Gallbladder hydatid disease is very rare which can be primary and secondary. In our case, It’s assumed that the daughter vesicles in gallbladder were secondary to primary hepatic hydatid cyst ruptured to biliary duct.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Birch S, Tyson E. An Extract of Two Letters from Mr. Sampson Birch, an Alderman and Apothecary at Stafford, concerning an Extraordinary Birth in Staffordshire, with Reflections Thereon by Edw. Tyson M. D. Fellow of the Coll.of Physitians, and of the R. Society. Phil Trans 1683 13, doi: , published 1 January 1683. [PubMed]
- Pedrosa I, Saíz A, Arrazola J, et al. Hydatid disease: radiologic and pathologic features and complications. Radiographics 2000;20:795-817. [PubMed]
- Erzurumlu K, Dervisoglu A, Polat C, et al. Intrabiliary rupture: an algorithm in the treatment of controversial complication of hepatic hydatidosis. World J Gastroenterol 2005;11:2472-6. [PubMed]
- Dew H. Some complications of hydatid disease. Br J Surg 1936;18:275-93.
- Lewall DB, McCorkell SJ. Rupture of echinococcal cysts: diagnosis, classification, and clinical implications. AJR Am J Roentgenol 1986;146:391-4. [PubMed]
- Alper A, Ariogul O, Emre A, et al. Choledochoduodenostomy for intrabiliary rupture of hydatid cysts of liver. Br J Surg 1987;74:243-5. [PubMed]
- Dadoukis J, Gamvros O, Aletras H. Intrabiliary rupture of the hydatid cyst of the liver. World J Surg 1984;8:786-90. [PubMed]
- Moguillanski SJ, Gimenez CR, Villavicencio RL. Radiologia de la hidatidosis abdominal. Radiologiae imagen diagnostica terapeutica: Abdomen. Vol 2. Philadelphia, Pa: Lippincott Williams & Wilkins 1999:47-72.